Prerenal causes
Children are particularly susceptible to prerenal failure. Normally the kidneys are able to maintain glomerular filtration in the face of a fall in arterial blood pressure, through a process of renal autoregulation. This is dependent on preglomerular vasodilation. The main reasons for impairment of this autoregulatory process in children are renal artery stenosis or ACE-inhibitor therapy. If the blood pressure continues to fall, these compensatory mechanisms fail and GFR falls.
Agents causing renal vasoconstriction can lead to renal failure, even in the presence of a normal blood pressure. These include a number of vasoactive agents used in paediatric intensive care, such as noradrenaline and high dose dopamine. Endotoxaemia may cause renal vasoconstriction, despite peripheral vasodilation.
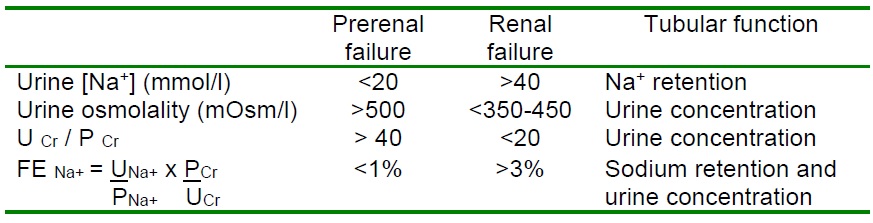
It is important to recognise prerenal failure as prompt administration of fluids may restore renal function, while excess fluid in the presence of established renal failure is hazardous. Management of such children in the intensive care setting can be aided by the monitoring of central venous pressure, as assessment of volume status is notoriously difficult in children. In the prerenal state tubular function should be intact and renal vasoconstriction causes sodium retention and a concentrated urine (see table). Administration of a limited fluid challenge should lead to a diuretic response.
Indices aiding in the differentiation of prerenal and renal failure.